The prognosis for Peritoneal Mesothelioma begins with the accepted reveal of the patient's medical history to settle symptoms and any past asbestos exposure, as well as a complete physical. In addition, sometimes physicians might request an Mri (magnetic resonance imaging) scan or an X-ray of the abdomen or chest region to help settle the location and size of the tumor. In an Mri, a powerful magnet connected to a computer is used to make detailed pictures of areas inside the body. These pictures are viewed on a monitor and can also be printed, clearly depicting the areas affected with the tumor.
In cases of pleural and peritoneal mesothelioma, fluid (effusion) may derive in the chest or abdominal region. In such cases, physicians may use a course known as fine needle aspiration to derive a sample of this fluid for supplementary testing. In addition, this course can be used to drain the effusion to temporarily ease chest pain or other painful symptoms.
Lung Aspiration
Usually, a biopsy of the tumor is required to confirm a prognosis of mesothelioma, however, sometimes only an effusion sample is needed. Some of the procedures ordinarily used for the prognosis of the peritoneal mesothelioma contain peritoneoscopy, thoracoscopy, and biopsy. With peritoneoscopy, the doctor will use a tool called a peritoneoscope, which is placed inside an occasion made in the patient's abdomen. Fluid, if found, is then drained; the process of draining the fluid is called paracentesis, and it requires a needle to be placed inside the abdomen in order to excerpt the fluid.
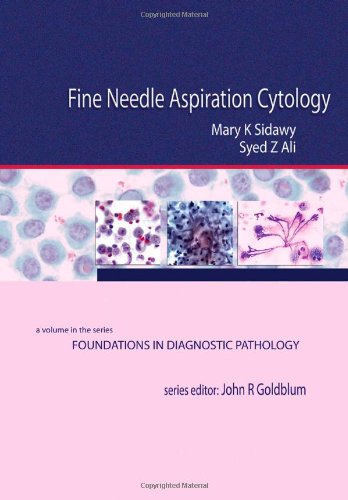
Fine Needle Aspiration Cytology: A Volume in Foundations in Diagnostic Pathology, 1e Best
Rate This Product :

Fine Needle Aspiration Cytology: A Volume in Foundations in Diagnostic Pathology, 1e Overview
Expansively illustrated, this volume in the "Foundations in Diagnostic Pathology" series encompasses aspiration cytopathology of all major body sites. Experts in the field provide you with a clear, concise, and practical diagnostic approach to the challenges you face every day. Color photomicrographs provide a visual image of individual lesions, to make learning quick and easy. The consistent, convenient format provides quick, at-a-glance reference, making it an excellent resource not only for the pathologists-in-training but for those in practice as well.- Uses highly templated chapters to make key information easy to find.
- Incorporates carefully selected high-quality, full-color images.
- Covers aspiration cytopathology of all major body sites.
- LIncludes contributions from the world's preeminent cytopathologists.
The Foundations in Diagnostic Pathology Series answers the call for fresh, affordable, and easy-to-use guidance. Each region-specific volume provides all of the most essential information on the pathologic entities encountered in practice. Series Editor: John R. Goldblum, MD, FACP, FASCP, FACG
Customer Reviews
*** Product Information and Prices Stored: Mar 20, 2012 02:19:26
In thoracoscopy a doctor uses a extra instrument called a thoracoscope in order to seek the patient's chest cavity. An incision is made in the chest wall, and the thoracoscope is placed in the middle of the patient's ribs. If the fluid is found in the chest, the doctor drains it from the chest cavity through a needle. A thoracoscopy ordinarily requires an anesthetic or some other form of pain suppression.
In a biopsy, if cancerous tissue is found in the patient's lungs or abdomen it will be extracted and examined by the doctor. This process helps the doctor settle potential ways of medicine and is commonly done during one of the other two processes or may want supplementary surgery.
Peritoneal Mesothelioma diagnosisHigh Definition Imaging of the GI Tract-Mayo Clinic Video Clips. Duration : 13.87 Mins.Just as cameras and televisions have been reinvented in the last decade with improved optics, sharpness and brightness, so have the tiny imaging scopes that physicians use to peer into the bodys nooks and crannies — its organs and digestive system. Researchers at the Florida campus of Mayo Clinic are testing the power of these new endoscopic optics to potentially help prevent or detect early colon cancer, lung cancer metastasis, and esophageal cancer. Results of a number of these studies, led by Michael Wallace, MD, MPH, professor of medicine, are being presenting at the annual international scientific conference, Digestive Disease Week (DDW) 2010. In one study, for example, gastroenterologists at Mayo have pitted multiple high-tech probes against each other to see how well they detect the tiniest precancerous polyp in the colon. They have determined that one endoscopic imaging tool called the probe-based confocal laser endomicroscopy (pCLE) shows the highest accuracy yet in detecting small precancerous polyps inside the colon wall. The probe is only one-sixteenth of an inch in diameter. We can see detail that was unimagined 10 years ago, says Dr. Wallace. We can zoom in on a potential problem spot in the colon with 1000-fold magnification, leading to a day when we can perform virtual biopsies on patients meaning that we will be able to tell if a lesion is precancerous by looking at it, and if it isnt, we can leave it alone. Now we have to remove anything that looks even ...
Tags: Mayo Clinic, Endoscopy, High Definition, Imaging, Wallace